Chorion villus sampling
What is chorion villus sampling?
Chorionic villus sampling is an invasive test that involves sampling and examination of the chorionic villi from the placental tissue.
Why it is done and to whom is this test offered?
Chorionic villous sampling (CVS) is offered to pregnant women who have a higher risk of having a baby born with a chromosomal or genetic abnormality. Every pregnant woman has this risk regardless of her age, family history or ethnic background although, it increases with advanced maternal age or if there is a family history of an underlying genetic abnormality.
What are chromosomes and genes?
Chromosomes are thread-like strands composed of DNA and are located within each cell in our body. They are responsible for containing the instructions that carry hereditary information in the form of genes. As the genetic material passes from parents to child, the chromosomes are responsible for containing the Instructions that make the offspring unique while still carrying traits from the patient.
About 2 or 3 out of a hundred pregnancies (2-3%) will be affected by a birth defect. Birth defects can have many causes, including chromosome or genetic abnormalities. We usually have 46 chromosomes, 23 pairs, in the cells that make our bodies. We inherit one of each pair from our mother, the other one from our father. Chromosomes carry thousands of genes. Genes determine how a baby develops, looks and how the body functions. Having extra or missing chromosome material or a change in an important gene can interfere with a baby’s development. Many of these conditions happen out of the blue around conception. Sometimes, conditions can be inherited.
How and when is CVS done?
The test is usually done between 11-14 weeks of pregnancy.
It is performed under local anaesthesia and a fine needle is passed through the mother’s abdomen under ultrasound guidance to obtain a sample of placental tissue for analysis. The procedure usually takes around 5 -10 minutes to perform and the fetal heartbeat is shown to the mother after the procedure. The sample is then checked to ensure if adequate villi have been obtained for analysis. A repeat test may be performed if the sample was found to be inadequate on examination.
What are the side effects and risks of CVS?
While most of the women tolerate the procedure well, some might expect pain and discomfort for which paracetamol can be taken. It is usually advisable to take rest following procedure and can resume normal activity the following day.
The risk of miscarriage is less than 0.5 % (1 in 200 procedures) following CVS and is characterised by bleeding, leaking water through the vagina and/or fever for which we would recommend urgent medical advice and hospitalisation. This risk is usually higher for 2-3 days after the procedure.
What happens next?
The samples will be sent to the genetics laboratory for analysis. The timing of results would depend on the nature of the test and will be informed to the parents accordingly. The parents need to be aware that in around 1% of the cases, the laboratory would not be able to culture the cells from the sample and hence the test may have to be repeated.
Once the results are available, the couple would be called to discuss the findings with a management plan. A copy of the results with our recommendations and follow up will also be sent to your Doctor.
Amniocentesis
What is amniocentesis:
Amniocentesis is an invasive test that involves sampling of the amniotic fluid which contain fetal cells.
Why it is done and to whom is this test offered?
Amniocentesis is offered to pregnant women who have a higher risk of having a baby born with a chromosomal or genetic abnormality. Every pregnant woman has this risk regardless of her age, family history or ethnic background although, it increases with advanced maternal age or if there is a family history of an underlying genetic abnormality. The cells in the amniotic fluid originate from the fetus; hence the chromosomes would be that of the baby inside the womb.
What are chromosomes and genes?
Chromosomes are thread-like strands composed of DNA and are located within each cell in our body. They are responsible for containing the instructions that carry hereditary information in the form of genes. As the genetic material passes from parents to child, the chromosomes are responsible for containing the Instructions that make the offspring unique while still carrying traits from the patient.
About 2 or 3 out of a hundred pregnancies (2-3%) will be affected by a birth defect. Birth defects can have many causes, including chromosome or genetic abnormalities. We usually have 46 chromosomes, 23 pairs, in the cells that make our bodies. We inherit one of each pair from our mother, the other one from our father. Chromosomes carry thousands of genes. Genes determine how a baby develops, looks and how the body functions. Having extra or missing chromosome material or a change in an important gene can interfere with a baby’s development. Many of these conditions happen out of the blue around conception. Sometimes, conditions can be inherited.
How and when is Amniocentesis done?
The test is usually done after 15 weeks of gestation onwards. Most women, however, prefer it to have it done before 20 weeks.
Under constant ultrasound guidance, a fine needle is passed through the mother’s abdomen to obtain a sample of the amniotic fluid which is then sent for analysis. The procedure usually takes around 5 -10 minutes to perform and the fetal heartbeat is shown to the mother after the procedure. Amniotic fluid is mainly fetal urine which reaccumulates within a few hours.
What are the side effects and risks of Amniocentesis?
While most of the women tolerate the procedure well, some might expect pain and discomfort for which paracetamol can be taken. It is usually advisable to take rest after the procedure and can resume normal activity the following day.
The risk of miscarriage is less than 0.5% (1 in 200 procedures) following amniocentesis and is characterised by bleeding, leaking water through the vagina and/or fever for which we would recommend urgent medical advice and hospitalisation. This risk is usually higher for 2-3 days following the procedure.
What happens next?
The samples will be sent to the genetics laboratory for analysis. The timing of results would depend on the nature of the test and will be informed to the parents accordingly before leaving the unit. The parents need to be aware that in around 1% of the cases, the laboratory would not be able to culture the cells from the sample and hence the test may have to be repeated.
Once the results are available, the couple would be called to discuss the findings and management plan. A copy of the results with our recommendations and follow up will also be sent to your Doctor.
Fetal blood sampling (FBS)
What is Fetal blood sampling?
Fetal blood sampling also known as cordocentesis is an invasive test that involves sampling of the fetal blood.
Why it is done and to whom is this test offered?
Fetal blood sampling is primarily used to diagnose fetal anaemia. In addition, it could also be used to check for congenital fetal infections (e.g parvovirus) and for chromosomal and genetic abnormalities.
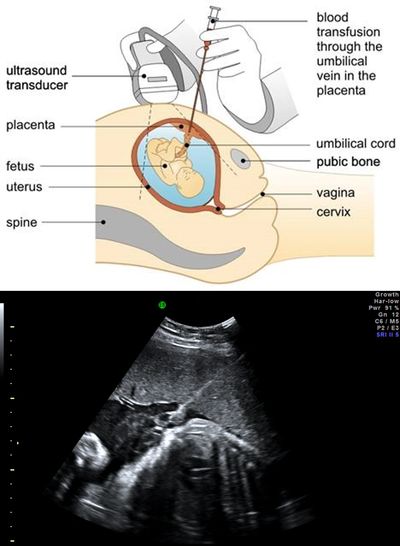
Following fetal blood sampling, the same needle entry could be used for intrauterine fetal blood transfusion and injecting medications as part of fetal therapy.
How and when is FBS done?
FBS is usually performed as early as 18 weeks onwards in pregnancy.
Under local anaesthesia and constant ultrasound guidance, a fine needle is passed through the mother’s abdomen to obtain a sample of the fetal blood from the umbilical cord close to the placental cord insertion avoiding sampling from the free loop of cord. Alternative sites for FBs include Intrahepatic portion of the umbilical vein in the fetus. The procedure usually takes 10-15 minutes and the fetal heartbeat is shown to the mother at the end of the procedure.
What are the side effects and risks of cordocentesis?
While most of the women tolerate the procedure well, some might expect pain and discomfort for which paracetamol can be taken. It is usually advisable to take rest after the procedure and can resume normal activity the following day.
The risk of miscarriage is around 1% (1 in 100 procedures) after cordocentesis. In addition, there is a small risk of adverse outcome including fetal demise.
What happens next?
The samples will be sent to the laboratory for analysis. The timing of the results would depend on the nature of the test and will be informed. The parents need to be aware that in around 1% of the cases, we would not be able to obtain results due to technical factors and hence the test may have to be repeated.
Once the results are available, the couple would be called to discuss the findings and management plan. A copy of the results with our recommendations and follow up will also be sent to your Doctor.
Fetal blood transfusion
Fetal tissue biopsy
What is fetal tissue biopsy?
This is a procedure to obtain fetal tissue /skin samples under ultrasound guidance for analysis. This is usually done between 17-20 weeks of gestation under local anaesthesia. The procedure usually takes around 5-10 minutes to perform and samples will be sent to the genetic laboratory for further analysis.

Genetics

