Multifetal pregnancy reduction (MFPR)
What is Multifetal pregnancy reduction (MFPR)?
Multifetal pregnancy reduction (MFPR) is a procedure to reduce the number of fetuses in higher-order multiple pregnancies (Triplets and above).
There has been a substantial increase in high order multiple pregnancies (Twins, Triplets, and Quadruplets) as a result of the surge in assisted reproductive techniques over the last two to three decades.
Despite significant improvements in expected management, the risks of miscarriage and preterm delivery remain higher with significant risks of prematurity associated with a greater number of fetuses inside the womb. In addition, there is also an increased risk of maternal complications that occur in women having more babies in the womb.
These risks are further complicated when they have an identical (monochorionic) pair as they contribute to an additional risk of developing twin to twin transfusion syndrome that requires fetal therapy.
Numerous published studies have shown that MFPR is associated with a significant reduction of the risk of preterm delivery without a significant increase in the risk of miscarriage when compared to conservative management.
How and when is MFPR done?
MFPR is usually done between 12 to 16 weeks. The method of fetal reduction depends on the type of multiple pregnancy which would be discussed with the couple after the scan. The procedure is done under local anaesthesia and is usually done as a day care procedure. Patients are usually sent home after a few hours following treatment; However, occasionally they may have to be admitted overnight in hospital for observation.
What are the side effects and risks of MFPR?
The risk of miscarriage is around 2% following the procedure although this would very much depend on the clinical case and complexity of the twins. The doctors will have an extensive counselling with the couple before they decide to undergo the treatment.
What happens next?
The pregnancy will be closely monitored for the next 2 weeks to observe if there are any complications following the procedure. If normal, they can be discharged to continue their care with their obstetrician. A copy of the report will also be sent to her obstetrician with the suggested management plan and follow up.

Multifetal pregnancy reduction(MFPR)
Intrauterine transfusion (IUT)
Intrauterine Blood transfusion (IUT):
An intrauterine transfusion is a procedure which involves transfusing blood to a fetus usually through the umbilical cord or via the intrahepatic portion of the umbilical vein. It is used to treat fetal anaemia commonly occurring due to red cell alloimmunisation when fetal blood cells are being destroyed by maternal antibodies. In addition, its also used to treat fetal anaemia due to congenital infection (e.g. parvo virus), feto maternal haemorrhage and Twin anaemia Polycythaemia sequence to name a few.
What are the risks associated with IUT?
Although the procedure is generally considered safe to perform, fetal distress during or after the procedure can occur that may result in intrauterine death of the fetus. In addition, there is also an increased risk of preterm delivery with risks of prematurity associated with early delivery. This could range anywhere between 1-5% depending on the indication and the complexity of the procedure.
Fetoscopic laser ablation (FLAP)
What is FLAP?
In twins sharing the same placenta (Monochorionic twins), there are blood vessels that run along the surface of the placenta establishing connection between the two umbilical cords. In most of the cases, the blood flow between the vessels do not cause any harm to the pregnancy. However, in around 15% of these twins, there is an imbalance of blood flow between the fetuses giving rise to a condition called Twin to Twin Transfusion syndrome or TTTs. If this condition gets severe, we must stop the blood flow between the twins by using laser.
When is FLAP done?
FLAP is usually done between 16-26 weeks of pregnancy when the risk is higher in the twins to develop TTTs.
How is FLAP done?
FLAP is performed under local anaesthesia. A 3mm calibre fetoscope (like laparoscope) is introduced through the mother’s abdomen into the uterus. The blood vessel which are seen to divert blood from one fetus to other are identified and blocked using Laser. This procedure helps in preventing the blood going from one fetus to another and help improve the condition. The procedure takes approximately 30-45 minutes to perform depending on case complexity. After the procedure, the mother is admitted overnight for observation and discharged the next day.
What are the risks and benefits of doing Laser?
Currently, this is the only treatment available for TTTs to help both twins survive the pregnancy. The outcome depends on stage of TTTs and the complexity of the procedure with good double survival rates for early stage TTTs (around 70-75%). The risks include miscarriage (5%), demise of one or both fetuses (5-10%) despite treatment and the risk of neurological injury (6-8%) to one or both twins.
What happens next?
The pregnancy is closely monitored for complications that may occur during the next 2 weeks and if normal they can then be monitored according to the routine monochorionic twins by fortnightly scans. We would recommend a fetal MRI of the brain in 3-4 weeks to check for any evidence of injury following Laser. We would closely liaise with her obstetrician to arrange for further follow up and management.
Radio Frequency Ablation (RFA) /Microwave ablation
What is RFA?
Radiofrequency ablation is a method used for fetal reduction in twins (monochorionic twins) sharing the same placenta in the womb. The procedure is performed under local anaesthesia and usually takes around 30 minutes to perform depending on the case complexity. RFA is usually performed around 16 weeks of gestation. Patients are usually able to get back home the same day although some may require overnight admission for observation.
What happens next?
The pregnancy is closely monitored for complications that may occur during the next 2 weeks and if normal can then be monitored as routine. We usually recommend a fetal MRI of the brain in 3-4 weeks after the procedure to check for any evidence of injury following treatment. We would closely liaise with her obstetrician to arrange for further follow up and management.

Fetal tumour therapy
What are fetal tumours?
Fetal tumours are characterised by abnormal growth in the baby which can develop from a range of tissues. While majority of them can be small and benign, some may outgrow to harm the fetus. Large tumours can also cause significant shunting of blood from fetal circulation resulting in fetal heart failure and hydrops. The prognosis depends on the underlying cause, location and additional abnormalities.
How are fetal tumours treated?
Fetal tumours are treated by blocking the blood supply either by Radiofrequency ablation or Laser which can result in the reduction of the size of the tumour. Some tumours can obstruct the airways which would require special delivery techniques, and this can be discussed with the couple prior to delivery.
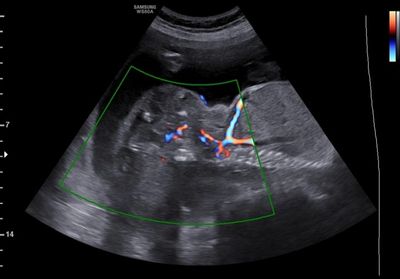
Large Sacrococcygeal teratoma with vascularity
Fetal shunts
What are fetal shunts?
Fetal shunts are intrauterine procedures done as part of fetal therapy in relieving either obstruction or draining fluid within the body cavities.
As each procedure differs in technique and complexity, we shall individually discuss in detail the benefits and risks of each procedure.

Fetal Thoracic shunt for pleural effusion

